

Nutrition and Respiratory Allergies: The Complete Evidence-Based Guide to Reducing Symptoms, Strengthening Immunity, and Improving Lung Health
Introduction
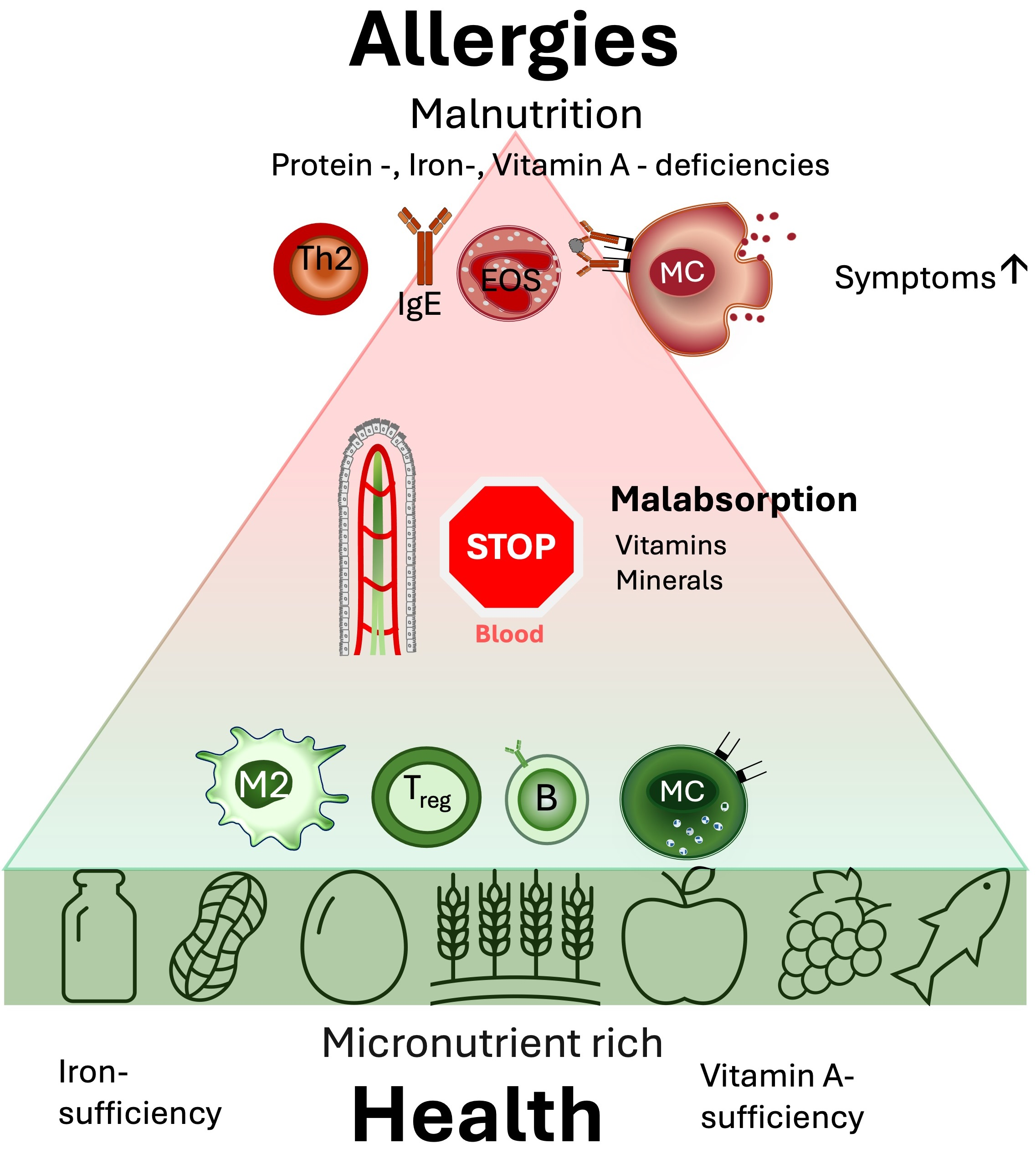
Respiratory allergies are among the most widespread chronic health conditions worldwide, affecting hundreds of millions of children and adults. Allergic rhinitis, asthma, and environmentally triggered breathing disorders are no longer viewed solely as problems of pollen, dust mites, or air pollution. Over the past two decades, scientific research has revealed a powerful and often underestimated factor in respiratory allergy development and severity: nutrition.
Nutrition does far more than provide energy. It shapes immune responses, influences inflammation, alters gut microbiota, and even affects how our lungs react to allergens. Poor dietary patterns—high in ultra-processed foods, refined sugars, and unhealthy fats—are increasingly linked to higher allergy prevalence and more severe respiratory symptoms. Conversely, nutrient-dense diets rich in antioxidants, fiber, healthy fats, and specific micronutrients appear to protect lung tissue and modulate allergic reactions.
This comprehensive, expert-level article explores the deep and complex relationship between nutrition and respiratory allergies, offering a science-based, practical roadmap for patients, clinicians, nutritionists, and health-conscious readers. You will learn how food affects immune tolerance, which nutrients support respiratory health, which foods may worsen allergic symptoms, and how to design a long-term dietary strategy to improve breathing and quality of life.
Understanding Respiratory Allergies: A Nutritional Perspective
What Are Respiratory Allergies?
Respiratory allergies occur when the immune system overreacts to harmless airborne substances, known as allergens. These allergens include pollen, mold spores, pet dander, dust mites, and air pollutants. In sensitized individuals, exposure leads to an exaggerated immune response, releasing inflammatory mediators such as histamine, leukotrienes, and cytokines.
Common respiratory allergic conditions include:
-
Allergic rhinitis (hay fever)
-
Allergic asthma
-
Exercise-induced bronchoconstriction
-
Occupational respiratory allergies
Traditionally, treatment focuses on allergen avoidance and medication. However, nutrition plays a crucial upstream role by influencing immune sensitivity, inflammation thresholds, and lung resilience.
Why Nutrition Matters in Respiratory Allergies
The immune system does not operate in isolation. It is deeply interconnected with metabolism, the gut microbiome, and nutritional status. Key reasons nutrition matters include:
-
Immune modulation: Nutrients regulate immune cell differentiation and inflammatory signaling.
-
Oxidative stress control: Antioxidants protect airway tissues from allergen-induced damage.
-
Gut–lung axis: The gut microbiota, shaped by diet, communicates with the lungs and influences allergic responses.
-
Inflammation balance: Dietary fats and sugars can either promote or suppress chronic inflammation.
Understanding these mechanisms helps explain why dietary interventions can reduce symptom severity even when allergens remain present.
بعوضة النمرفي العالم والجزائر: خصائصها ومخاطرها وطرق مكافحتها
كيف تعزز مناعتك ضد العدوى الفيروسية؟
Top Superfoods: Nature’s Most Powerful Foods for Health, Energy, and Longevity
Kombucha: Benefits, Brewing, Science & Safety
25فائدة تجميلية للكفير أو الفطر الهندي
The Gut–Lung Axis: Where Nutrition and Respiratory Allergies Meet
The Gut Microbiome and Immune Tolerance
One of the most revolutionary discoveries in allergy research is the gut–lung axis. The gut microbiome—trillions of microorganisms living in the digestive tract—plays a decisive role in immune education.
A diverse, balanced microbiome promotes immune tolerance, reducing the likelihood of allergic sensitization. Diets rich in fiber, fermented foods, and plant diversity nourish beneficial bacteria that produce short-chain fatty acids (SCFAs), such as butyrate. These compounds help regulate immune responses and reduce airway inflammation.
In contrast, diets high in processed foods and low in fiber reduce microbial diversity and are associated with increased asthma and allergic rhinitis risk.
Early Nutrition and Allergy Risk
Nutrition during pregnancy, infancy, and early childhood strongly influences respiratory allergy risk later in life. Evidence suggests:
-
Maternal diets rich in fruits, vegetables, and omega-3 fatty acids reduce asthma risk in children.
-
Breastfeeding supports healthy microbiome development and immune regulation.
-
Early introduction of diverse foods may reduce immune hypersensitivity.
These findings emphasize nutrition as both a preventive and therapeutic tool.
Inflammation: The Core Link Between Diet and Respiratory Allergies
Chronic Inflammation and Allergic Airways
Respiratory allergies are fundamentally inflammatory conditions. When allergens enter the airways, immune cells release inflammatory mediators that cause:
-
Nasal congestion
-
Bronchoconstriction
-
Mucus overproduction
-
Coughing and wheezing
Diet strongly influences baseline inflammation levels. A pro-inflammatory diet primes the immune system for exaggerated responses, while an anti-inflammatory diet can reduce symptom intensity.
Pro-Inflammatory Dietary Patterns
Certain dietary habits are consistently associated with worse respiratory outcomes:
-
High intake of refined carbohydrates and sugary beverages
-
Excessive omega-6 fatty acids from processed vegetable oils
-
Low consumption of fruits and vegetables
-
Frequent fast-food consumption
These patterns increase oxidative stress and inflammatory cytokine production, worsening airway sensitivity.
Key Nutrients That Support Respiratory Allergy Management
1. Antioxidants and Respiratory Protection
Antioxidants neutralize free radicals generated during allergic inflammation. The lungs are particularly vulnerable to oxidative damage due to constant exposure to oxygen and pollutants.
Key antioxidants include:
-
Vitamin C: Supports immune balance and may reduce bronchial hyperreactivity.
-
Vitamin E: Protects airway cell membranes from oxidative stress.
-
Carotenoids: Found in colorful fruits and vegetables, associated with better lung function.
-
Polyphenols: Present in berries, green tea, and olive oil, known for anti-allergic effects.
Regular consumption of antioxidant-rich foods is associated with reduced asthma symptoms and improved respiratory resilience.
2. Omega-3 Fatty Acids and Inflammation Control
Omega-3 fatty acids play a central role in regulating inflammatory pathways. They compete with pro-inflammatory omega-6 fatty acids and lead to the production of specialized pro-resolving mediators.
Benefits for respiratory allergies include:
-
Reduced airway inflammation
-
Improved lung function
-
Lower medication dependence in some individuals
Dietary sources include fatty fish, flaxseeds, chia seeds, and walnuts. Balancing omega-3 and omega-6 intake is more important than simply increasing fat consumption.
3. Vitamin D and Immune Regulation
Vitamin D deficiency is common worldwide and has been strongly associated with increased asthma severity and allergic rhinitis frequency.
Vitamin D influences respiratory allergies by:
-
Regulating immune tolerance
-
Reducing inflammatory cytokine release
-
Supporting epithelial barrier integrity in the lungs
Adequate vitamin D status is associated with fewer asthma exacerbations and better symptom control, particularly in individuals with chronic respiratory allergies.
4. Magnesium and Bronchial Relaxation
Magnesium is involved in smooth muscle relaxation and nervous system regulation. In respiratory allergies and asthma, magnesium may help reduce bronchoconstriction and improve airflow.
Low magnesium intake has been linked to:
-
Increased airway hyperresponsiveness
-
Higher asthma prevalence
-
More severe respiratory symptoms
Foods rich in magnesium include leafy greens, nuts, seeds, whole grains, and legumes.
5. Zinc and Immune Balance
Zinc supports immune cell development and antioxidant defenses. Deficiency may impair immune regulation and increase susceptibility to infections that worsen respiratory allergies.
Adequate zinc intake contributes to:
-
Reduced infection-induced asthma attacks
-
Improved mucosal immunity
-
Balanced inflammatory responses
Foods That May Worsen Respiratory Allergies
Histamine-Rich and Histamine-Releasing Foods
Histamine is a central mediator of allergic symptoms. Some foods naturally contain histamine or stimulate its release, potentially worsening respiratory allergy symptoms in sensitive individuals.
Common examples include:
-
Aged cheeses
-
Processed meats
-
Fermented alcoholic beverages
-
Certain fish products
While not everyone is sensitive, individuals with histamine intolerance may notice increased nasal congestion, wheezing, or headaches after consuming these foods.
100 سؤال وجواب حول التغذية والسمنة
التغذية والأمراض العصبية دليلك الشامل
التغذية وهشاشة العظام:دليلك الشامل
التغذية وأمراض القولون:دليلك الشامل
تغذية مرضى السيلياك:100 سؤال وجواب
Food Additives and Preservatives
Artificial additives, sulfites, and preservatives can trigger asthma symptoms in susceptible individuals. Sulfites, in particular, are known to provoke bronchospasm in some people with asthma.
Reducing consumption of highly processed foods can significantly improve symptom control.
Obesity, Overnutrition, and Respiratory Allergies
Excess body weight is a recognized risk factor for asthma severity and poor respiratory outcomes. Adipose tissue produces inflammatory mediators that amplify allergic inflammation and impair lung mechanics.
Weight-balanced nutrition supports:
-
Improved lung capacity
-
Reduced systemic inflammation
-
Better response to allergy medications
Dietary Patterns That Support Respiratory Health
The Mediterranean Diet and Allergies
The Mediterranean diet is one of the most studied dietary patterns in allergy research. It emphasizes:
-
Fruits and vegetables
-
Whole grains
-
Olive oil
-
Fish and legumes
This diet provides antioxidants, fiber, and healthy fats that collectively reduce inflammation and support immune balance. Studies consistently associate Mediterranean-style eating with lower asthma prevalence and better respiratory outcomes.
Plant-Forward Diets and Allergy Protection
Plant-rich diets increase fiber intake and microbial diversity, supporting the gut–lung axis. They also reduce intake of pro-inflammatory saturated fats.
However, careful planning is required to ensure adequate intake of nutrients such as vitamin B12, iron, and zinc.
Elimination Diets: Benefits and Risks
Some individuals with respiratory allergies explore elimination diets to identify food triggers. While short-term elimination may help in specific cases, unnecessary long-term restriction can lead to nutrient deficiencies.
Professional guidance is essential when considering elimination diets for respiratory allergy management.
Nutrition Strategies for Specific Respiratory Allergic Conditions
Allergic Rhinitis
Nutritional strategies focus on reducing histamine release and supporting mucosal health. Antioxidant-rich foods, adequate hydration, and omega-3 intake are particularly beneficial.
Allergic Asthma
For asthma, dietary goals include reducing airway inflammation, improving lung mechanics, and preventing obesity. Balanced macronutrient intake and micronutrient sufficiency are critical.
Practical Meal Planning for Respiratory Allergy Support
Daily Nutritional Priorities
An allergy-supportive diet should include:
-
A wide variety of fruits and vegetables
-
Adequate protein from lean and plant sources
-
Healthy fats from fish, nuts, and olive oil
-
Whole grains for fiber and microbiome health
Hydration and Mucus Management
Adequate hydration helps maintain optimal mucus viscosity, making breathing easier and reducing congestion.
Nutrition, Lifestyle, and Environmental Synergy
Nutrition works best when combined with:
-
Regular physical activity
-
Adequate sleep
-
Stress management
-
Reduced exposure to indoor and outdoor pollutants
This holistic approach addresses respiratory allergies at multiple biological levels.
Emerging Research and Future Directions
Research continues to explore personalized nutrition, microbiome-targeted therapies, and nutrigenomics in respiratory allergy management. Future dietary recommendations may become increasingly individualized based on genetic and microbial profiles.
Conclusion
The relationship between nutrition and respiratory allergies is complex, powerful, and scientifically undeniable. Food choices influence immune tolerance, inflammatory balance, lung function, and symptom severity. While nutrition is not a replacement for medical treatment, it is a foundational pillar of comprehensive respiratory allergy management.
By adopting an anti-inflammatory, nutrient-dense dietary pattern and avoiding known triggers, individuals with respiratory allergies can significantly improve their breathing, reduce symptom burden, and enhance overall quality of life. Nutrition transforms respiratory allergy care from reactive symptom control into proactive, long-term health optimization.






